A permanent pacemaker is a small electronic device that helps your heart maintain a regular, healthy rhythm. It’s implanted in your chest to regulate electrical problems with the heart, such as beating too quickly or too slowly.
This guide tells you how pacemakers work, what happens during a pacemaker operation and the potential risks and complications.
Why is a permanent pacemaker needed and how does it work?
You may need a pacemaker if you have a heartbeat that’s too slow or too fast, or is irregular. Pacemakers are also used to treat conditions such as congestive heart failure and hypertrophic cardiomyopathy.
Normally, the heart beats when electrical impulses stimulate the heart muscle and make it contract. One part of your heart, called the sino-atrial node, releases electrical pulses which make the heart contract and pump blood to the ventricles, and in turn to the lungs and body.
If your heart has a problem that interferes with those regular electrical impulses, or the “timing” of those electrical impulses is interrupted, you will need a permanent pacemaker.
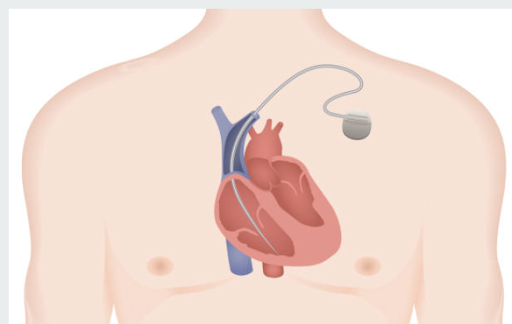
A pacemaker sends regular electrical signals to the heart, helping it pump at a normal, healthy rate. It’s a small battery-powered box that’s implanted into the chest permanently, with small, insulated wires that deliver electrical impulses to your heart. After surgery, the pacemaker sits under the skin near the heart, on either the left or right side of your chest.
Pacemakers are commonly used for anyone with heart rhythm problems, and help your heart maintain a healthy heartbeat.
A pacemaker may help you regain a more active, healthy lifestyle if your heart problems have affected your life. Often patients report feeling more energetic after having a pacemaker implant.
Are there different types of pacemakers?
There are also temporary or short-term pacemakers, which stay outside your body. Temporary pacemakers are attached to the heart muscle through a small “pacing” wire via a vein or through the chest.
A temporary pacemaker is used to stabilise your heart rate in the short term. This might be needed because of physical trauma, infection, after a heart attack or heart surgery, or while you’re waiting for a permanent pacemaker.
If you have long-term problems with your heart, however, you may need a permanent pacemaker.
What are the signs that I might need a pacemaker?
You may need a permanent pacemaker if you have disturbances in your heart’s rhythm. Your heart may beat too quickly or too slowly, or may be irregular (which is known as an arrhythmia).
If you have problems with your heart rhythm, you might have symptoms such as:
- dizziness
- fatigue
- feeling short of breath
- fainting
If you’re seeing a cardiologist because you have an arrhythmia, you won’t necessarily need a pacemaker. There are different types of arrythmias, many of which are harmless and don’t need to be regulated with a pacemaker to restore the rhythm.
Your doctor will discuss the best treatment options for you depending on the type of arrhythmia you have.
How do pacemakers work and differ?
There are a few different types of pacemakers, and your doctor will decide which one is right for you. Pacemakers have either one, two or three leads, depending on your individual heart problem.
The main types are:
- Single chamber: One lead connecting to one upper or lower chamber of the heart.
- Dual chamber: Two leads connecting to one top and one bottom chamber.
- Biventricular: Three leads connecting to the right atrium, right ventricle and left ventricle. This pacemaker is often used to treat advanced heart failure.
What are the potential risks of a permanent pacemaker procedure?
While permanent pacemakers are common, as with any medical procedure there are some potential risks and complications. These include:
- infection at the site of the incision
- swelling, bruising or bleeding
- blood clots near the pacemaker
- blood vessel damage
- collapsed lung
- movement of the leads
While there are some potential risks, a pacemaker implant is generally a safe procedure. If you’re worried or concerned, talk to your doctor.

Our expert team will look after you during every stage of your permanent pacemaker procedure
What happens during pacemaker surgery?
Before surgery, your doctor will discuss what medications you’re taking and whether you need to stop or change anything.
Talk to your doctor about whether you need to stop taking any medication. Read more about medication and fasting, but don’t stop or change any medications until you have spoken to your doctor.
Before your permanent pacemaker surgery, you’ll be attached to a heart monitor and have a drip inserted into your arm. You’ll be given medication to provide pain relief and help you relax.
The surgery will take place in an operating theatre. Once an incision is made near the collarbone, the pacemaker leads are threaded into a large vein on the right side of your heart, and fixed inside the heart using tiny screws.
Your surgeon will program the pacemaker and test it during the procedure. The pacemaker will then be put under the skin, and the incision will be stitched and a dressing applied.
You’ll be at the clinic for six to eight hours from admission to discharge. The surgery itself takes about one hour. However, you may need to stay at the clinic overnight, and if that’s the case, your doctor will discuss this with you.
What do I need to do afterwards?
After the procedure, you won’t be able to drive for 24 hours, so you’ll need to arrange for someone to take you home afterwards.
You also won’t be able to drive for about two weeks after having a pacemaker implanted.
After pacemaker surgery, it’s important to avoid driving. Your doctor will need to make sure that the leads are fixed in the right position and haven’t moved.
About six weeks after the implant surgery, you’ll need to have a follow-up appointment with your doctor to check the pacemaker.
Does life change after getting a pacemaker?
Having a pacemaker won’t change your life in any major way, but there are a few things to keep in mind.
Your pacemaker will regulate your heart’s rhythm, but it won’t stop heart disease or plaque building up in your arteries.
It’s still very important you look after your general health: keep up regular physical exercise, eat a healthy diet, avoid smoking and enjoy alcohol in moderation.
Here are some general rules about what you can and can’t do when you’re living with a pacemaker:
- You’ll need to have regular checks, usually once a year. The pacemaker will be checked wirelessly or via Bluetooth, so this won’t be invasive. The battery will also be checked. The pacemaker batteries will last between five and 15 years and your doctor will let you know well in advance when it will need changing.
- It’s a good idea to carry a card in your wallet or bag stating that you have a pacemaker, in case of emergency.
- If you need to have any further surgery, tests or scans, let your healthcare professionals know that you have a pacemaker. MRIs and CT scans can interfere with a pacemaker.
- Avoid putting your mobile phone in a pocket near your chest, and when you’re talking on a mobile hold the phone to the ear on the opposite side to the pacemaker.
- Keep away from electrical generators and high-voltage equipment such as welding equipment.
- Your pacemaker may trigger security alarms at airports, so let security staff know that you have one.
- Tell your doctor if your job involves operating heavy machinery or driving.
- Your pacemaker won’t affect whether you can play sport or have sex. Be wary of any high contact sports, though.
About Sutherland Heart Clinic
Sutherland Heart Clinic is a major interventional cardiology centre uniquely co–located
within Sutherland Hospital at Caringbah. The clinic offers a wide range of procedures including diagnostic studies, angioplasty procedures (with stents) and pacemaker procedures.
Learn more about our clinic, cardiology procedures, and what to expect if you’ll be visiting Sutherland Heart Clinic for a procedure.
Read more:

Recent Comments